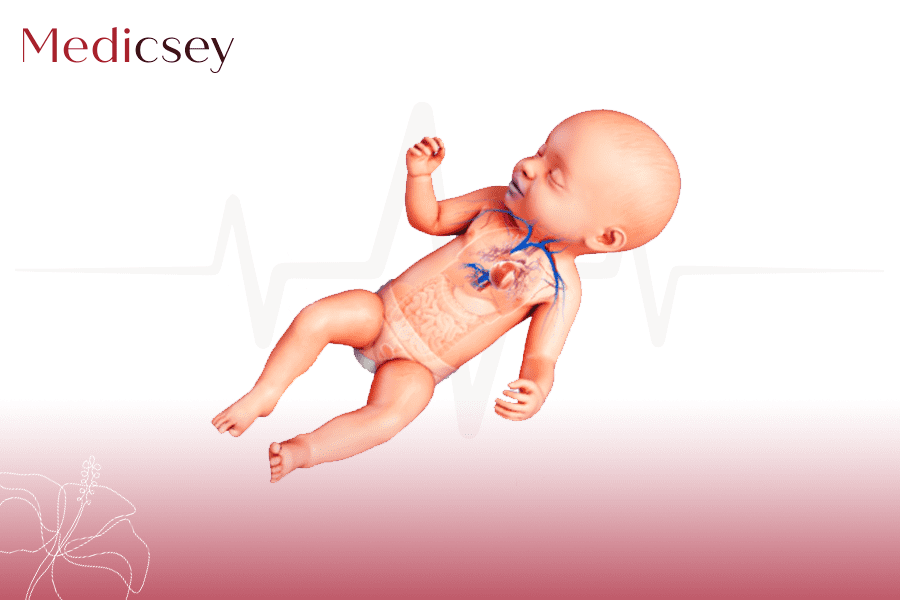
CONGENITAL BIRTH DEFECTS ( ASD & VSD )
Atrial and ventricular septal defects are among the most common heart birth defects.
Atrial septal defects (ASD) are located between the heart's upper chambers (atria), which receive blood from the body.
Ventricular septal defects (VSD) are located between the lower chambers (ventricles), which pump blood to the body.
These holes typically cause left-to-right shunting of blood, which means that some blood that has already picked up oxygen from the lungs goes through the hole and back to the lungs. This shunting is inefficient, and the extra blood flow to the lungs can cause symptoms.
Some atrial septal defects are actually just a stretched out foramen ovale (normal hole between the upper chambers that is present before birth). Most of these defects patent foramen ovale close on their own within the first 3 years of life, although sometimes they persist into adulthood. A true hole between the atria (true atrial septal defect) usually does not close.
Ventricular septal defects can be located in several different sections of the wall between the lower chambers of the heart. Some have a good chance of closing on their own (for example, those that are called muscular ventricular septal defects) whereas others do not close spontaneously.
Septal Defect: A Hole in the Heart's Wall
|
A septal defect is a hole in the wall (septum) that separates the heart into the left and right sides. Atrial septal defects are located between the heart's upper chambers (atria). Ventricular septal defects are located between the lower chambers (ventricles). In both types, some oxygenated blood, intended for the body, is shortcircuited. It is returned to the lungs rather than pumped to the rest of the body. |
Symptoms
Atrial septal defects
Infants and children with atrial septal defects usually have no symptoms. Once in a while, a child with an atrial septal defect will grow slowly.
However, in early adulthood or middle age, atrial septal defects that are untreated, particularly those that are large, can lead to a stroke and/or high blood pressure in the lungs (pulmonary hypertension ). Even smaller atrial septal defects can become more serious over time as the left side of the heart naturally stiffens, pushing more blood through the hole and back through the lungs.
Ventricular septal defects
Ventricular septal defects can vary from small holes, which may cause a heart murmur but no symptoms, to larger holes that cause symptoms early in life. Symptoms due to larger ventricular septal defects usually develop when a infant is between 6 and 8 weeks of age and include rapid breathing, difficulty feeding, sweating while eating, and slow weight gain. These symptoms suggest the child is developing heart failure.If untreated, children may also have recurrent lung infections and increased pressure in the lung blood vessels (pulmonary hypertension) that will eventually become permanent, leading to numerous complications and shortened life span.
Sometimes, a VSD is close enough to the aortic valve that it affects the valve. The affected aortic valve may start to leak (called aortic regurgitation). With aortic regurgitation, some blood that was pumped out flows back into the heart . Aortic regurgitation can cause heart failure if not treated.
Diagnosis
- Echocardiography
Doctors often suspect a septal defect if they hear a certain kind of heart murmur. A heart murmur is a sound created by turbulent blood flow through narrowed or leaking heart valves or through abnormal heart structures.
For both atrial and ventricular septal defects echocardiography (ultrasonography of the heart) is done to confirm the diagnosis and determine the size and location of the defect and any associated enlargement of heart chambers. Echocardiography will also show if other heart defects are present.
Electrocardiography (ECG) is typically done, even in infants. ECG may show signs that one or more heart chambers are enlarged. Chest x-rays may show an enlarged heart.
Treatment
- Sometimes drugs, a plug or other specialized device inserted through a catheter, or surgery
Treatment depends on the type and size of the defect and whether it is causing symptoms.
Atrial septal defects
Because atrial septal defects usually cause no symptoms, affected children do not usually need any drugs. If the hole persists beyond age 2 to 3 years, unless the hole is tiny, doctors usually recommend closure to prevent complications. Atrial septal defects that are located in the center of the wall between the upper chambers can often be closed during a procedure done in the cardiac catheterization laboratory. During this procedure, a long thin tube (catheter) is inserted into the large vein at the top of the child's leg and then carefully pushed up through the blood vessel until it reaches the heart. Once the catheter is in the proper location, the closure device is threaded through the catheter and out of the tip of the catheter, allowing the device to expand and seal the hole.
Atrial Septal Defect Repair
ASDs that are very large or located at the edges of the atrial septum usually need to be closed surgically with a patch.
Some children need to take antibiotics before visits to the dentist and before certain surgeries (such as on the respiratory tract). These antibiotics are used to prevent serious heart infections called endocarditis.
Ventricular septal defects
Children with small ventricular septal defects usually require no treatment. However, some smaller VSDs located near the aortic valve can cause the valve to leak (aortic regurgitation). If children have aortic regurgitation, doctors usually do surgery to close the VSD and sometimes repair or replace the aortic valve.
Infants with symptoms related to moderate or large VSDs may first be treated with drugs, such as furosemide (a diuretic, which pulls excess fluid out of the body), digoxin (to help the heart to pump more forcefully), and/or an angiotensin-converting enzyme (ACE) inhibitor (to relax blood vessels and help the heart to pump more easily). These drugs help relieve symptoms and allow time for the VSD to close on its own. If symptoms do not improve or the VSD does not get smaller, doctors usually do surgery to close the VSD.
Certain types of VSD can sometimes be closed with a catheter device but this is less likely to be appropriate than with ASDs.
Ventricular Septal Defect Patch
Some children need to take antibiotics before visits to the dentist and before certain surgeries (such as on the respiratory tract). These antibiotics are used to prevent serious heart infections called endocarditis.








.webp)


.webp)

.webp)